In modern medicine, the objective is not just to treat patients, but also to improve their well-being and QoL, hence the increasing interest in research on social support and QoL experienced by patients with a variety of conditions. Such a comprehensive assessment is especially important in patients who have lost a pregnancy, as this experience entails a number of consequences, not only physical, but also psychological and social, and at times, even financial. Each patient has her own needs and beliefs that affect her individual perception of her health and living situation. Therefore, we undertook to evaluate the levels of QoL, social support, and self-efficacy in this patient group [16,17].
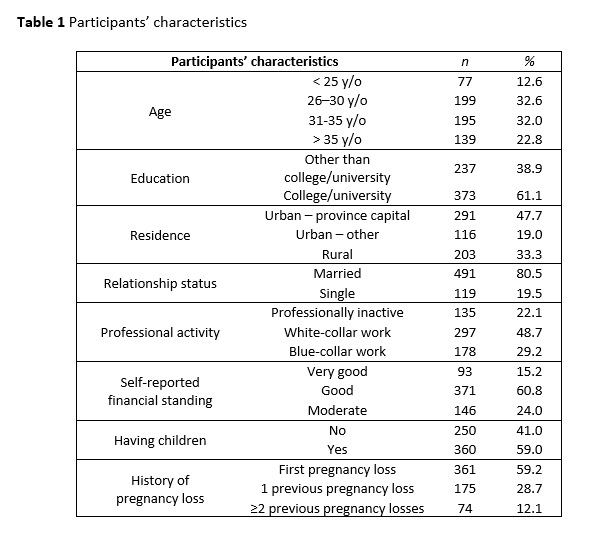
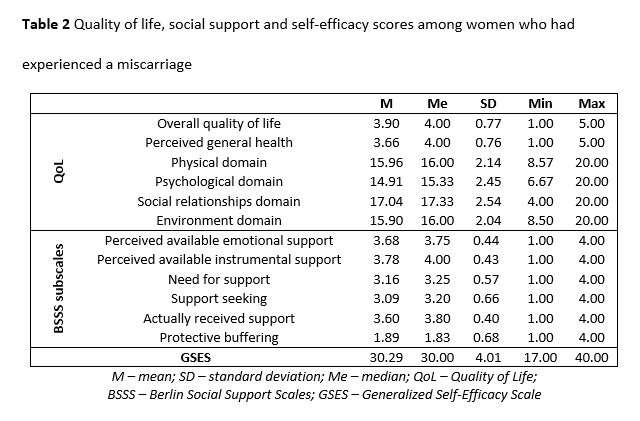
Our findings are to some extent consistent with those reported by other researchers studying the subject. Like patients with hyperglycemia in pregnancy and those treated for polycystic ovary syndrome, the women who have experienced a miscarriage who were studied rated their overall QoL higher than their overall perceived health [22,23].
The social relationships domain was scored highest, as was the case in studies by Couto et al. and Tavoli et al. regarding women after pregnancy loss [24,25]. The high scores in the physical domain were also consistent with the report by Tavoli et al. [25]. Interestingly, in the QoL self-assessment by physically active women during uncomplicated pregnancy, the scores in the physical domain were next to lowest, while the highest scores were reported in the psychological domain [26]. In the present study, women who had lost a pregnancy reported lower QoL in the psychological domain. Respondents’ psychological well-being was also rated lower than other QoL aspects in the studies by Couto et al. and Tivoli et al., although these authors placed more emphasis on the limitations in the performance of social roles, associated with emotional difficulties [24,25]. In turn, Song et al., analyzing the long-term effects of a child’s death on the parents, reported much poorer QoL than in the case of non-bereaved individuals [27]. Other authors also highlighted considerable differences in QoL between pregnant subjects with no history of obstetric problems and ones after a pregnancy loss, with the latter group having lower QoL [24,25,28,29].
QoL is also significantly associated with social support, which is a major contributor to a patient’s health and treatment success [15]. In the group of women who have miscarried, perceived available support, both instrumental and emotional, and actually received support was rated highly. The present statistical analysis findings are comparable to those reported by Iwanowicz-Palus G. et al. in a group of patients with hyperglycemia in pregnancy [22].
The association between social support and satisfaction with life was previously demonstrated e.g. by Strine et al. in their US study. They found that overall dissatisfaction with life increased as the level of social support decreased [30]. Gul et al. (2018), Emmanuel et al. (2012) and Shishehgar et al. (2013) also reported a positive correlation between social support and QoL in pregnant women [31,32,33].
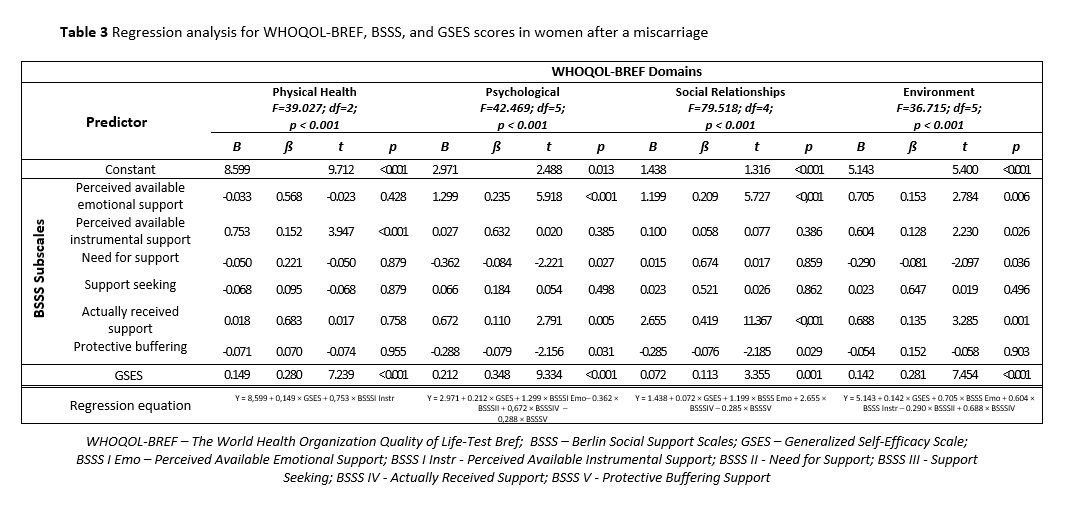
A literature review demonstrates that social bonds have a beneficial impact on various aspects of an individual’s psycho-physical condition, including reduced health-related stress, anxiety, and depressive symptoms [30,33,34,35,36,37]. The results of the present study indicate an association between perceived available emotional support and actually received social support, on the one hand, and better QoL in the psychological domain on the other. The quality of social support received from various sources and the professional demeanor of medical personnel also affect the patient’s psychological well-being and satisfaction with life.
Pregnancy loss is a stressful event that may prompt a psychological crisis [7,9]. The process of coping with a difficult health-related situation is shaped by a number of factors, one of which is self-efficacy [11]. A literature review does not reveal many reports on the subject in the field of gynecology. It is, however, a highly consequential topic, as an individual’s expectations and beliefs have a significant impact on their actions, as well as on their physical and psychological health [11,13,38].
The patients who had experienced a miscarriage and who participated in our survey had a higher level of generalized self-efficacy than that found in a standardization group for the Polish population, which was moderate (this included women with pregnancy complications, post-menopausal women, diabetic patients, patients on dialysis, and patients with a history of myocardial infarction) [11]. This suggests that the patients studied here were involved in their treatment process and actively coping with their difficult situation. Similar results were found in groups of patients who had had a mastectomy and pregnant women with hyperglycemia [11,22].
Self-efficacy may affect QoL or satisfaction with life. It is also one of the cognitive factors that affect the way individuals manage stress [11,12,13,19].
The available publications suggest that building self-efficacy by strengthening a patient’s sense of control and ability to manage a given life situation may counteract negative emotions or exacerbations of depressive symptoms [39,40,41,42]. An analysis by Nikcevic et al. demonstrated a significant association between more self-efficacy and less anxiety and depression in women who had lost a pregnancy [38]. The present analysis confirms the impact of self-efficacy on all QoL domains in the women studied , and the strongest positive correlation was found for the psychological QoL domain.
As pregnancy loss may have negative psychological health consequences, it is worth considering strategies to enhance self-efficacy, especially among women found to have lower levels of this resource [5,8,9,10]. The present findings may contribute to a better understanding of care involving not just professional medical interventions, but also the provision of adequate social support. Providing support and improving the self-efficacy of women after pregnancy loss seem extremely important for patients’ psycho-social well-being and QoL, on a level with effective medical management. In practice, these aspects should be included among the priorities of medical personnel’s daily work.
Strengths and limitations of the study
The strengths of our study include the sample size (610 patients) and personal communication with each respondent. As we used standardized instruments, other researchers interested in issues related to pregnancy loss will be able to compare results, continue in-depth research and monitor changes. The available studies on women who have had a miscarriage were typically performed weeks or months after the event. We investigated patients during hospitalization, as this is when the coping process typically begins.
One difficulty was associated with the personal administration of surveys to the respondents, as during their 3–6 days of hospitalization, they also underwent multiple intensive diagnostic and treatment procedures. Therefore, to ensure the highest possible quality and reliability of our study, information on the stage of treatment, duration of hospitalization, and the clinical condition of the patient was obtained from medical personnel before contact with each patient. The study instrument was given to each patient on the last day of her hospitalization, having ascertained that her treatment had been completed and her psycho-physical condition had been stabilized.
One limitation of the present study is the lack of data on the QoL of women with a normal pregnancy course until week 22, against which we could compare the scores found in women after pregnancy loss.
Our study is limited by its cross-sectional design, as it does not allow for identifying any causal relationships between quality of life, social support and self-efficacy in women who have had a miscarriage.