Results
Study participants
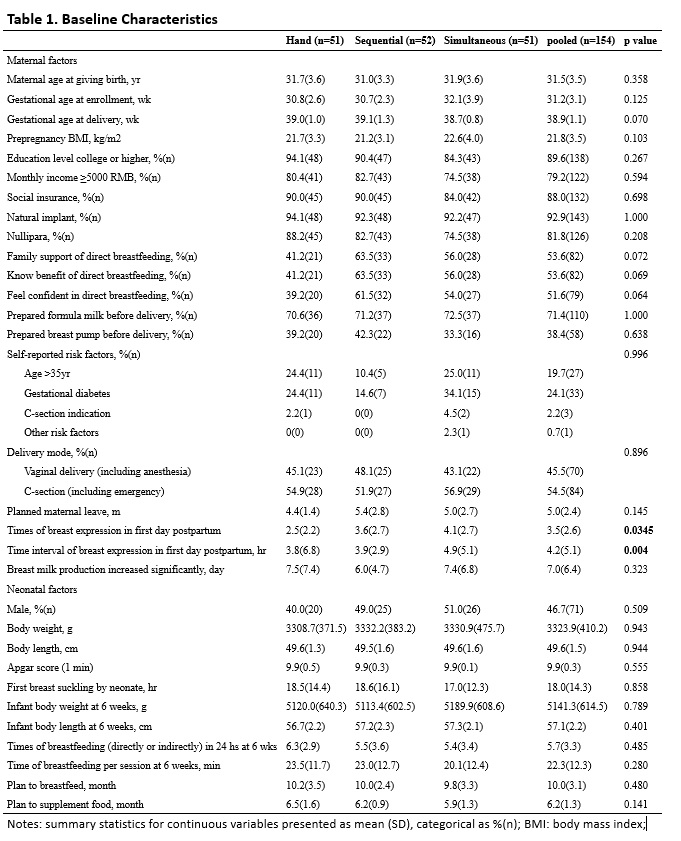
Following prenatal examination 226 participants returned written informed consent. After delivery 2/3 of them (n=154) were randomized into the three trial groups of breast expression. Six participants withdrew between hospital discharge and review at 6 weeks. Meanwhile 2 participants stopped breastfeeding prematurely due to maternal health problems. Later, over 20% participants declined feedback at 4 months though they remained in contact. At 6 months less than half of participants in total remained in contact. More participants were lost to follow-up during the last 2 months than in previous 4 months, especially in group of sequential breast expression (Figure 1). The three groups were well balanced at baseline (Table 1).
Primary outcomes
The estimated median times required for breastfeeding initiation of hand expression, sequential breast pumping, and simultaneous breast pumping were 46.7 (95% CI 40.8-50.0), 46.5 (95% CI 36.1-50.5) and 45.6 (95% CI 34.2-53.0) hours, respectively. In each of the three groups, around 10% participants initiated breastfeeding after 3 days (i.e., >72 hr). Compared with hand expression, sequential and simultaneous breast pumping did not promote earlier initiation of breastfeeding (log-rank test, p=1.000) (Figure 2A). For dyads with vaginal delivery, the median time to breastfeeding initiation with simultaneous breast pumping was 34.2 (95% CI 26.9-53.0) hours, with sequential pumping is 45.3 (95% CI 20.3-49.0) hours, and with hand expression 45.7 (95% CI 31.4-51.8) hours. For dyads in which cesarean section had been used, the median times to initiation with breast pumps were somewhat longer - 49.3 (95% CI 38.9-66.8, p=0.096) hours for simultaneous pumping and 50.5 (95% CI 40.2-67.1, p=0.086) hours for sequential pumping. However, the differences were not statistically significant (Figure 2B). With regard to mode of delivery, the time required for breastfeeding initiation in women with vaginal delivery was significantly less (median 45.1 (95% CI 31.4-48.0) hours) than for women who had cesarean section (median 48.2 (95% CI 43.5-53.0) hours; p=0.002) (Figure 2C).
The efficacy of breast expression in the early and mature stages of lactation was measured through expressed breast milk volume. The breast milk volume was estimated from weight, either of test weighing in the hand expressing group at 3 days or 6 weeks, or of weights in two breast pump groups at 3 days when the milk volume was <10 ml. At 3 days after birth the infants in hand expression group were breastfed directly and weighed right before and after feeding. Averaged breast milk volumes were 23.8±26.2 ml for hand expression, 16.7±11.6 ml for sequential pumping and 13.1±10.9 ml for simultaneous pumping. Averaged breast milk volume in simultaneous pumping was less than that in hand expression group through direct breastfeeding (p=0.007). However, it was not different from that for sequential pumping (p=0.560). There was no difference between two delivery modes (vaginal delivery vs cesarean section) and no difference in subgroups of delivery mode in three groups (Figure 3A).
At 6 weeks the averaged breast milk volumes in a 10-minute session were 89.8±67.3 ml for hand expression, 64.7±51.0 ml for sequential pumping and 71.6±50.8 ml for simultaneous pumping.. The average breast milk volume in the sequential pumping group was statistically significantly less than that of the hand expression group (p=0.035) but was not different from that of the simultaneous pumping (p=0.670). The averaged breast milk volume at 6 weeks were 72.8±55.1 ml in participants with vaginal delivery and 71.8±55.0 ml in these who underwent cesarean section; the difference was not statistically significant (p=0.834),. Further subgroup analysis of breast milk volume of delivery modes in three groups did not show any statistical difference (Figure 3B). The average milk volume from the left breast was about 2 ml less than that from the right breast (p=0.012).
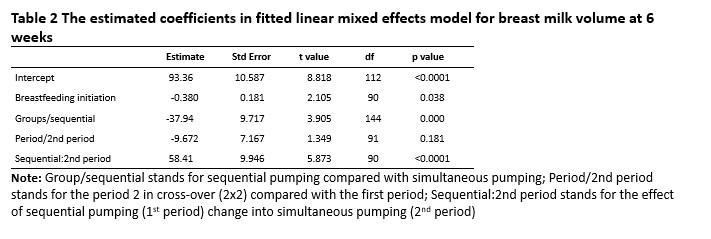
To minimize random effect from individual woman, cross over of the two breast pump types by two periods (2×2) was applied at 6 weeks. In the 1st period (before breast pump cross over) the average breast milk volumes of sequential and simultaneous pumping groups were 40.4±25.3 ml and 76.5±52.5 ml (p=0.001), respectively. In 2nd period (after breast pump cross over) the averaged breast milk volumes of sequential and simultaneous pumping groups were 88.6±58.3 ml and 67.0±49.7 ml (p=0.167), respectively. Total breast milk volume pumped in 1st period (59.3±45.0 ml) was less than that in 2nd period (79.0±55.1 ml) (p=0.009). The increase in breast milk volume associated with transition from sequential to simultaneous pumping was statistically significant (p<0.001), while the converse transition from simultaneous to sequential pumping was not (Figure 4). A linear mixed effects model was fitted for this cross over design by using breast milk volume at 6 weeks as the dependent variable (Table 2).
Secondary outcomes
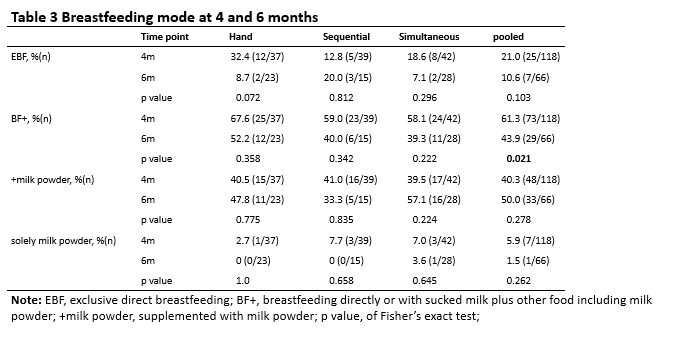
At 4 months, among women who completed the online questionnaire, the median count of self-reported direct breastfeeding sessions was 5.5 (interquartile range, IQR 2-8) per day, the median count of using breast pumps was 2 (IQR 2-4) sessions per day, and the averaged breast milk volume expressed at each session was 172.4±95.7 ml. In the following two months infant body weight increased by about 800 grams (p<0.0001) and body length increased by 3 cm (p=0.030) on average. The baby’s body weights differed between the three groups at six months (p=0.016) while their body lengths differed between the three groups at four months (p=0.033). In both breast pumping groups, 80% of mothers reported using the breast pumps frequently. Among participants who responded, 80.0% used breast pumps at 4 months and 71.9% at 6 months. The proportions were not different among three groups at 4 and 6 months (p=0.079, p=0.436), or by delivery modes (p=0.737). The paired student t test on expressed milk volume of mothers showed no difference (p=0.787) between 4 and at 6 months (pairs=41). The expressed breast milk volume in mothers who responded only once (at 4 months, n=35) was 136.8 ml, less than the 202.6 ml expressed by mothers who responded both (at 4 and at 6 months, n=41) (p=0.002). At 4 months, the maternity leave of 50.4% nursing mothers had ended, and this increased to 80.0% at 6 months (p<0.001). About 90% mothers provided complementary food to their infants at 6 months. The rate of introduction of formula milk was 40%- at 4, and 50% at 6, months. In terms of breastfeeding mode, the proportion of exclusive breastfeeding dropped from 21% at 4 months to 10% at 6 months. The rates of exclusive breastfeeding did not differ between the three groups either, at 4 months (p=0.109) or at 6 months (p=0.459) (Table 3).
Adverse events
No serious or severe adverse events episodes were reported in follow-up to six months. The proportion who reported any type of local breast adverse events was 11.5% and for any types of systemic adverse events of mild to moderate severity 2.9%. Eleven participants (one from the hand expression group, two from the sequential breast pump and eight from the simultaneous pump group) reported 12 local (breast) adverse events with mild to moderate severity. These local adverse events, which included breast skin rash, breast pain, breast lump or swelling, cracked nipple and slightly peeling of the areola, resolved without treatment. Three cases (one from the hand expression and two from the sequential breast pump group) reported fever, mastitis and antibiotics for high fever with moderate severity, all of which resolved after medical treatment.