Case Presentation
A 24-year-old male was complained of intermediate dry cough for one month. He denied any history of fever, weight loss, chest pain. Chest CT showed a tumor located on the posterior 6th left rib, which measured about 20 mm × 18 mm. An area of local bony destruction with conserved cortex was noted, and the margins were delineated with some ossifying matrix. Enhanced CT revealed non-uniform enhancement. There was no evidence of extension to the adjacent soft tissue. The imaging first diagnosis was LCH, a giant cell tumor, or other type of neoplasm. (Fig. 1)
His family medical history was negative for any type of malignancy. On physical examination, the tumor was not palpable and no pain by pressing on the chest wall. The overlying skin was normal, and no sensory deficit. Laboratory testing results, including tumor markers, complete blood cell count and erythrocyte sedimentation rate were within the normal range. The derivation purified protein skin test and tuberculosis test were negative.
VATS was used to resect the tumor and partial broken rib. It was observed to be present on the posterior side of the 6th left rib, the margins were well-defined, and no evidence of adjacent soft tissue invasion was noted. The tumor was resected from the rib, and broken cortical bone was noted. Frozen section pathological examination demonstrated a benign or a low-grade malignant bone tumor. Thus, the broken area of the rib including a margin of at least 10 mm of normal rib and adjacent partial intercostal muscle were resected. No reconstruction was required for the rib deficit. (Fig. 2)
Histopathological examination of hematoxylin and eosin (HE) stained revealed typical polygonal-shaped chondroblasts and osteoclast-like giant cells. The chondroblasts were large and closely packed with a central, characteristically translucent cytoplasm and grooved nucleus. (Fig. 3)
IHC examination made a diagnosis of chondroblastoma. (Fig. 4)
There were no intraoperative or postoperative complications, and the patient was discharged after five days. Patient described only minimal pain, and had only 2 small incisions on the chest wall. There was little impact on lung function, and a shorten chest drainage tube time and hospital stay. (Fig. 5)
Radical resection and no adjuvant therapy were given postoperatively. The patient was followed every 3 months with chest CT or chest radiograph and blood tests within the first year and every 4 months within the second year. The patient has no chest pain, chest tightness, shortness of breath, no abnormal breathing on the chest wall and the lung function is normal. About 23 months follow-up there is no evidence of recurrence or lung metastases.
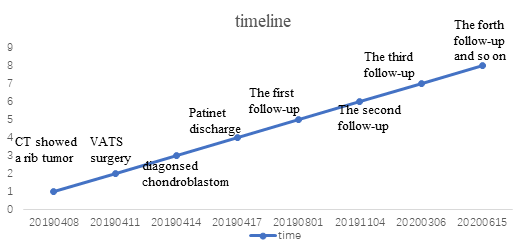
A timeline showed the whole medical procedure of this case.