The zygomatic bone is one of the pillars of the facial skeleton, having the role and the ability to absorb a large parts of the impact forces developed by a wounding agent [7]. However, when the kinetic energy developed is too high, the zygomatic bone will fracture either as a monoblock, becoming entirely detached from the midface, or in a comminuted manner [7,8] Depending on the mechanism, the type, the form, the consistency, the surface and the direction of the wounding agent multiple fracture patterns can occur at this level [7, 8]. In our study, complete fractures with zygomatic bone disjunction were predominant, a result supported by other authors as well [2,4-8]. Incomplete fractures are non-characteristic and rare in the zygomatic complex due to the reduced bone thickness secondary to maxillary sinus pneumatization [9]. In our study, all incomplete fracture lines were found in the temporo-zygomatic arch, either in association with complete anterior tripod fractures of the zygomatic bone or isolated. This result is confirmed in the literature by a number of authors [9-11]. It can be explained by the presence of the cortical bone which is better represented at this level, and also by the fact that the temporo-zygomatic arch can fracture through an indirect flexion mechanism, secondary to direct fracturing and primary inferomedial displacement of the zygomatic bone [10,11]. In this context, secondary to a low-kinetic energy trauma, the temporo-zygomatic arch fracture is either not synchronous with the anterior suture lines or incomplete [8]. Isolated temporo-zygomatic arch fractures are rare, their reported percentage in the literature ranging between 0.5 and 14% [3-5,9-11]. A solitary temporo-zygomaic arch fracture, requires a lateral and perpendicular impact direction to the face [10]. Given that the direction of action of wounding agents on the face is most frequently anterior or anterolateral, there are small chances that fractures will occur solely at this level [9-11].
The majority of the fractures in our study were displaced fractures, which is in accordance with the results of other authors [3-5,9-11]. Contrary to our results, some authors report an increased incidence of non-displaced zygomatic bone fractures [12], while others report a higher incidence of comminuted fractures [13,14]. Differences between the inclusion criteria in these studies may create the present divergences in the literature. We included exclusively patients with CT imaging investigations based on which we could easily identify minimal displacements of the fractured fragments. Minimal bone fragment displacements may go unnoticed on plain radiographs, the type of fracture being thus classified in a different category [12]. Biomechanically, displacement in the case of zygomatic bone fractures is primary, being directly proportional to the kinetic energy resulting from the impact, the type of the wounding agent and its direction of action [9-11]. Secondary displacement, following traction of the masseter muscle insertions, occurs rarely, having a reduced biomechanically importance [3]. Comminuted fractures occur in the context of strong traumas such as those from road traffic accidents, firearms or explosives [13,14]. In our study, the small number of comminuted fractures can be attributed to the fact that in our geographical area, injuries caused by interpersonal violence through fist blows are predominant [15]. It is well known that most of the times, the kinetic energy developed by fist blows is rarely sufficient to induce multiple fractures of the viscerocranium [16]. The predominance of injuries to the zygomatic bone through low kinetic energy in our geographical area also explains the high incidence of closed fractures, without communication with the external environment in this study. This is emphasized by the results of other authors [12-17]. The majority of intra-orally open fractures are due to the adherence of the mucoperiosteum to the zygomatic-alveolar ridge, mucoperiosteal laceration occurring secondarily to significant displacement at this level [3-5,9-11]. In contrast, Keller et al.[13] and Kittle et al.[14], in studies conducted in armed conflict zones, report a predominance of extra-orally open zygomatic bone fractures. The differences in the characteristics of zygomatic bone fractures depending on the studied population, can explain the divergences present in the literature.
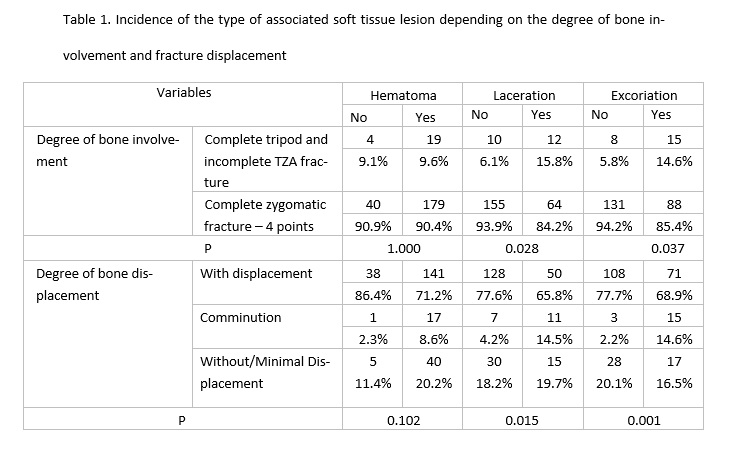
Hematoma was the most frequent associated soft tissue lesion in the current study, which is also reported by other authors [2,4,19,20]. Contrary to our results, other authors indicate the highest incidence of laceration [21, 22]. The fact that in the current study hematomas are predominant shows that the severity of the injuries included in this study is reduced.
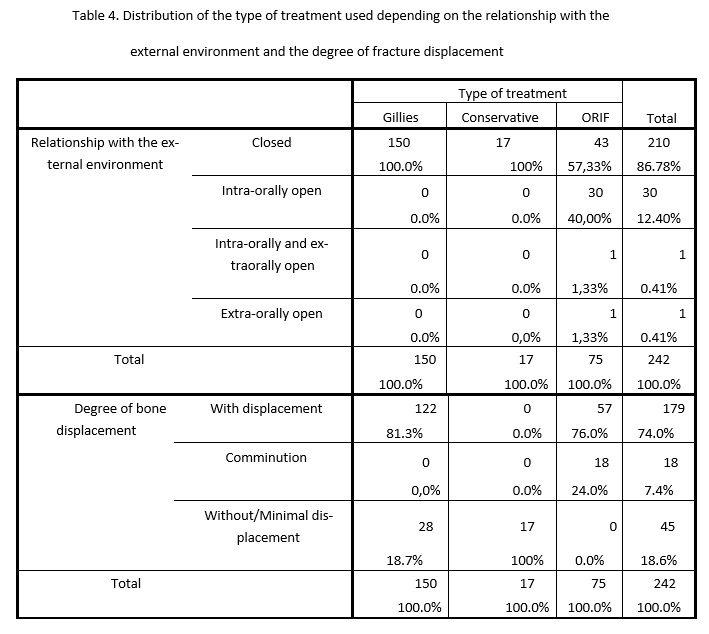
Gillies temporal approach reduction of the zygomatic bone was the most frequent therapeutic method used in our study, similarly to the results of other authors [2,23,24]. The great number of non-comminuted zygomatic fractures in this study explains this result. Although this method is losing ground to the new modern osteosynthesis techniques (ORIF), it can be useful and provide stable results over time in some cases [2]. The advantages of this method are rapid surgery, minimal scar masked by hair, minimal invasiveness, thus avoiding direct opening of the fracture foci, especially of the zygomatic-alveolar focus into the septic oral environment, and implicitly, the decrease in the risk of postoperative osteitis [2,33,34]. Another advantage that should not be overlooked is the decrease of hospital costs, the Gillies reduction involving no special materials or equipment, while the duration of hospitalization is minimum [2]. Despite all these advantages, the indications of this method are strictly limited to fractures with reduced displacement, with the integrity of the zygomatic fragment and maintenance of the periosteum on a sufficiently large surface at this level to ensure primary stability of the fractured bone [2,33,34].. This is also confirmed by the results of the current study. Some authors completely avoid using this method, saying that maintaining the perfect reduction of the bone fragments is impossible secondary to Gillies approach, which may have consequences over time [3,6,7,17,25]. Rana et al. [17] indicate the occurance of the zygomatic bone redisplacement at 6 weeks postoperatively following traction of the masseter muscle insertions during functional acts, in all patients in whom ORIF using 3 point fixation was not performed. Contrary to our results, other authors perform zygomatic bone fracture reduction by ORIF, considering it the treatment method of choice for this pathology [3,6,7,17,25-30]. ORIF of zygomatic bone fractures can be carried out using 1, 2, 3 or very rarely 4 point fixation [3]. We mention that in our study, ORIF was performed using 3 point fixation in all operated patients, according to the current protocol of the study host clinic. In contrast, globally, using the minimum number of fixation points is currently attempted to ensure zygomatic bone immobilization in order to reduce the risk of potential postoperative complications [3,4,7,9].. Forounzanfar et al.[7] and Kim et al.[29] present good results by using ORIF with 1 point fixation, the 3 point fixation of the zygomatic bone being rarely necessary. Czerwinski et al.[5,30] also report good results after using the endoscopically assisted ORIF-single incision technique. Correct reduction is systematically checked intraoperatively by fluoroscopy or computed tomography [5,6,30]. There is currently no consensus regarding the ideal number of fixation points in the case of zygomatic bone fractures, this aspect depending on the fracture pattern, surgeon’s experience and the available means [7].
In zygomatic bone fractures without displacement and without functional disorders, conservative treatment and follow-up of the patient are indicated, approach unanimously accepted in the literature [3,6,7,17,25-30]. Patient follow-up is absolutely necessary in this context [3,6,7,17,25-30]. Subsequent zygomatic bone displacement, either secondary to functional movements or due to novo trauma can occur, surgery being required under these conditions [3,6,7,17,25-30]. In our study, all cases in which conservative treatment was chosen had a favorable evolution. This shows that the indications of this method were entirely respected.
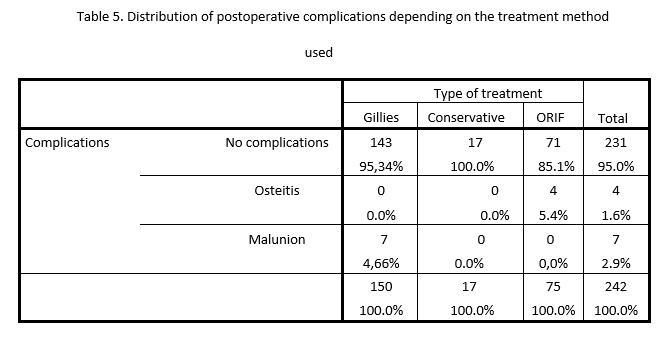
The most frequent postoperative complication was malunion, which occurred postoperatively in the case of Gillies reduction, in accordance with the results of other authors [7]. This result is not surprising given the inaccuracy of this method [9,17,19,26-28]. In contrast, other authors indicate an increased incidence of postoperative osteitis [3,28]. Osteitis in this study occurred only in 4 cases in the intra-oral osteosynthesis focus, probably due to bacterial contamination from the septic environment of the oral cavity. Removal of the osteosynthesis material under these circumstances led to a favorable result [9,17,19,26-28]. The persistence of infraorbital nerve sensory disturances postoperatively was not considered a postoperative complication in this study, it is known that post-traumatic sensory recovery can last up to 2 years or it may never occur. Also, the sensory disorders were not due to the surgical interventions, but being present clinically preoperatively. This fact is sustained also by other specialized studies [26-30].
The aim of this study was attained. The zygomatic bone fracture pattern and the interrelation between bone lesions and associated soft tissue lesions, as well as the most effective treatment were determined in a significant group of patients. Knowing the frequency of the association between a certain type of soft tissue lesion and a certain underlying zygomatic bone fracture pattern significantly contributes to a rapid and complete diagnosis, the maxillofacial surgeon knowing when to suspect the presence of a fracture masked by other clinical signs.
However, this study has a number of limitations. One of the most important limitations of the current study results from its retrospective nature; the data being collected from patients’ medical records, they might have been incomplete or incorrect. To minimize this drawback, only complete medical records were selected, but in this way, a number of cases from the statistical database were lost. Also the retrospective nature of study cannot allow the same inference as a randomized controlled trial. Therefore a randomized control trial regarding this subject is recommended in the future. Another limitation is the fact that in the midface, zygomatic bone fractures are frequently combined with orbital fractures, being difficult to evaluate retrospectively. Strictly including zygomatic bone fractures in this study resulted in the loss of a significant number of cases.