Methods
1.1 General Data
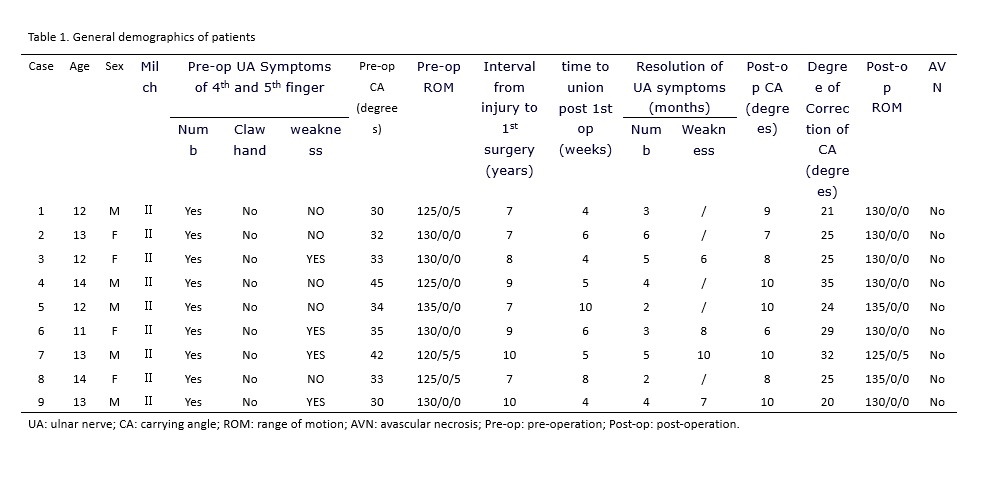
From January 2010 to January 2013, 9 older children (5 males and 4 females) aged average 12.7 years (ranged, 11-14 years) with humeral condylar fracture non-union old elbow valgus deformity were treated. Six were on the left side and three were on the right side. Interval from fractures to the first surgery ranged was 8.2 years on average (range, 7-10 years). The preoperative carrying angle was 35° on average (range, 30°-45°), with 7 cases between 30° and 40° while 2 between 40° and 50°. All patients showed ulnar nerve symptoms. Four cases had functional limitations in the 4th and 5th fingers, manifested by a mild weakness without obvious ulna claw deformity or any fixed deformities in the small joints. Elbow varus stress test showed a lateral instability of the affected elbow in all patients (Table 1).
1.2 Operation method
1.2.1 The first surgical stage was ORIF with bone grafting.
The patients lay on the operating table in a supine position with the affected arm abducted. A tourniquet was applied after induction of general anesthesia followed by skin preparation and draping. After inflation of tourniquet, a lateral longitudinal incision was made, 1/3 of which was distal to the humeroradial joint and 2/3 proximal to the humeroradial joint. The nonunion site of lateral condylar was visualized through the interval between triceps and brachioradialis which was retracted anteriorly and medially. The posterior soft tissue attachment of the fragment should be maintained in case of devascularization of the fragment. The outer periphery callus and fibrous tissue between the fragments were removed to refresh the fracture site, and the hardened bone on the fracture surface was also removed to expose the cancellous bone surface. The fragment was reduced with a point reduction forceps and temporarily fixed with Kirschner wires under direct vision to ensure the anatomic reduction of the fracture. If anatomic reduction was impossible, the fragment should be fixed at a position allowing the best elbow flexion and extension function. Then 4.0 mm diameter hollow screws were used as a final fixation, followed by allograft bone grafting. After the first surgery, a long arm plaster cast was applied to ensure a 90° elbow flexion and neutral position forearm. The cast was removed after 3 weeks. Three weeks after cast removal, functional activity training began.
1.2.2 The second surgical stage was correction of cubital valgus deformity.
Six months after ORIF of the nonunion, the previous internal fixators were removed and a supracondylar medial closing wedge osteotomy was carried out through the proximal part of the original lateral longitudinal incision. After the coronal plane deformity was corrected, the osteotomy was fixed with a lateral reconstruction locking plate and smooth Kirschner wires. External fixation with a cast was unnecessary after the second staged surgery, enabling the patient to begin elbow flexion and extension exercises the second day of recovery. After four weeks, if the elbow function was not fully recovered, patients were permitted to complete passive elbow flexion and extension activities under the guidance of doctors.