Materials And Methods
Participants
The study was conducted at the Department of Physical and Occupational Therapy, and the Department of Orthopedic Surgery, Horsens Regional Hospital (HRH), Denmark.
The study was conducted in accordance with the Declaration of Helsinki, and ethical approval was obtained from the Central Denmark Region Committee on Biomedical Research Ethics (journal number 1-10-72-166-18). Approval from the Danish Data Protection Agency (Journal number 1-16-02-90-18) was obtained and all patients gave written informed consent prior to inclusion.
Data were collected from April-July 2018.
Inclusion criteria were: Knee pain due to an orthopedic disorder, age ≥ 18 years, and ability to adhere for ≥ 4 weeks of twice-weekly LL-BFR.
Exclusion criteria were: cardiovascular diseases, former stroke, unregulated hypertension (systolic > 180 mmHg and/or diastolic > 110 mmHg), wound healing dysfunctions, former thrombosis, traumatic nerve injuries, renal insufficiency, varicose veins, diabetes, smoking, spinal cord injuries and pregnancy.
Eligible patients were referred to the study by orthopedic surgeons and collaborating physiotherapists at HRH. Also, patients diagnosed with knee Osteoarthritis (OA) not eligible for knee prosthesis were recruited at two OA seminars held at HRH.
Intervention
The training protocols applied in this project were designed based on available evidence and in collaboration with strength and conditioning coaches with practical experience in applying LL-BFR. In this study, supervised LL-BFR was performed twice weekly, with a minimum of one day between each session, for 4–8 weeks. Limb occlusion pressure (LOP) was determined as described by Ferraz et al. (7). LOP of the affected limb was determined at baseline for each patient.
Training Protocol
After 5 minutes of warm up on a stationary bike, patients performed one of two LL-BFR protocols (Table 1). Patients started each session on the affected limb. Subsequently, the non-affected limb performed the same amount of work as the affected limb (i.e. same cuff pressure, load). All sessions were supervised by a physiotherapist (SLJ) to ensure sufficient loading and progression.
Table 1: Exercise variables for the two BRFE protocols
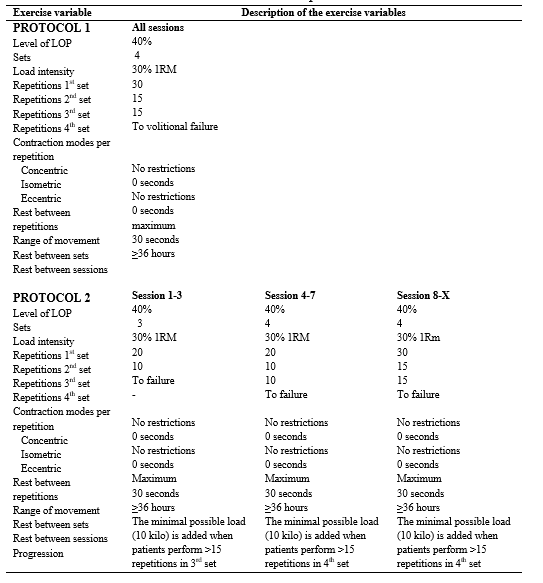
Table 1. Overview of the protocols used in the present study. A: no progression during the exercise period. B: Gradually progressing the training volume per session. Every third session, the volume was increased until reaching session number 8. From session 8, the training volume was kept constant.. LOP: Limb occlusion pressure; RM: Repetitions Maximum. The load was increased if the patients were able to perform more than 15 repetitions in the last set.
Outcomes
Adherence
At the first visit, the patients declared how many weeks they intended to participate which were used to calculate the adherence. Acceptable adherence to training was not defined a priory.
Descriptive measurements
Bodyweight, age, gender, and referring diagnosis were registered.
Baseline and follow-up tests
Prior to the physical tests at baseline and follow-up, patients completed the Knee Osteoarthritis Outcome Score (KOOS). KOOS is a patient-administered, knee-specific questionnaire comprising five subscales; Pain, Symptoms, activities of daily living (ADL), Sport & Recreation, and Knee-Related QoL (8). KOOS is responsive to change following non-surgical and surgical treatments of the knee (8).
Baseline tests were performed on the same day as the first LL-BFR session. Follow-up tests were performed on a separate day (~ 3 days after) after the last LL-BFR session.
The physical tests were executed chronologically as listed below:
Thigh circumference (TC) was measured with tape measure 10 cm above apex patella in supine on both limbs (9).
30-Seconds Chair Stand Test (30 s-CST) was used to determine the number of sit-to-stand repetitions a patient was able to complete within 30 seconds (10). The 30 s-CST was used to indicate lower limb strength and functional performance (10).
Timed Up & Go (TUG) was used to determine functional mobility and assess the time required for patients to stand from a chair (seat height 43 cm), walk around a tape mark 3 meters away, and sit onto the chair at return (11).
Maximum isometric contraction of the knee extensors (MVC Knee) was measured on both limbs with a hand-held dynamometer (HHD) (JTech Commander PowerTrack Muscle Dynamometer MMT, USA) as previously described in detail by Koblbauer et al. (12). Measurements were performed with the patient sitting on an examination table with knees and hips positioned at 90° flexion, and the HDD fixed with a rigid belt to the examination table (12).
1 Repetition maximum (1RM) leg press strength was estimated from a 5RM leg press test on the injured limb (13). The load was increased with 10–20 kilo until the patient could perform ≤ 5 repetitions. Two minutes rest was given between trials.
1RM was calculated as: 1𝑅𝑀 leg press (kg) = (1,1307·[5RM leg press (kg)]) + 0,66998) (14).
If a patient failed to perform a 5RM leg press test, the initial exercise loads was set to 20 kg.
Statistical analysis
Descriptive statistics are presented as means (standard deviation: SD) or medians with range. Normality was evaluated by plotting the data. Changes from pre- to post-intervention were evaluated using paired t-tests provided the assumption of normally distributed data was fulfilled. The Wilcoxon signed-rank test was used in cases where data did not follow normal distribution. If the result of parametric and non-parametric tests gave the same results, the results of parametric tests were presented. The level of significance was set at 5% (p ≤ 0.05). All statistics were performed in Stata (Stata/MP 16.1 for Windows). The purpose of the project was mainly to determine the feasibility of LL-BFR in patients suffering from lower limb injuries. Therefore, no power calculations for treatment effects were performed.