Methods
Study design and patients’ selection
This prospective cohort single-center study was approved by the Ethics Committee of the Institutional Review Board of Danang Family hospital, Danang, Vietnam (number: 12.04–30218), and written informed consent for procedures was obtained for all patients.
All patients were selected with the following inclusion criteria: (1) benign thyroid nodule(s) was confirmed by following recommendations from the Asian Conference on Tumor Ablation Task Force: US result and at least two separate US-guided fine-needle aspirations (US-FNAs) cytology or US-guided core needle biopsy (US-CNB) [19]; (2) reports of pressure symptoms (including pain, compressive symptoms, neck discomfort) or cosmetic problems, or anxiety about tumor; (3) refusal to undergo surgery. The exclusion criteria were as follows: (1) the largest dimension of the nodule(s) less than 15mm; (2) nodule(s) showing established or suspected malignant features during US (according to ACR-TIRADS 4 to 5) or cytology (according to Bethesda Class III to VI); (3) current thyrotoxicosis; (4) patients with short life expectancy by comorbidity of severe diseases; (5) pregnancy; and (6) patients lost to follow-up.
From January 2019 to October 2020, 93 patients who undergone treatment using the RFA were enrolled in this study
Measurement and assessment
Pre-treatment assessment and radiofrequency ablation procedure
Before the procedure, conventional clinical examination, US, 2 times separated US-guided FNAs or CNB, and the laboratory test was done. At registration, patients were evaluated for the compression symptoms using a 10-cm visual analog scale (0–10). Endocrinologist examined a cosmetic grade: 1, no palpable mass; 2, a palpable mass but no cosmetic problem; 3, cosmetic problem on swallowing only; 4, readily detected cosmetic problem [20]. An 8 to 12 MHz linear probe of a real-time ultrasound system (Acuson NX2 or NX3 series, Siemens Healthineer) was performed by only one radiologist with more than 5 years of experience. Nodule(s) was evaluated the position, size, volume, solid/cystic proportions, echogenicity, and volume (V = πabc/6 - where a, b, c are the 3 diameters). Ultrasound-guided FNA or CNB examinations were done by a licensed endocrinologist with more than 3 years of experience (Nguyen VB). Thyroid function (thyroid-stimulating hormone (TSH), free thyroxin (FT4) level) was obtained. Before the treatment of each patient, we explained the advantages and disadvantages of thyroid RFA.
All the procedures were performed by the same endocrinologist (Nguyen VB), who has a licensed certificate and more than 3 years of experience in US-FNA/CNB, thyroid ethanol ablation, and thyroid RFA, at the outpatient department of the Center of Endocrinology and Diabetes, Danang Family hospital, Vietnam. In the RFA procedure, patients in a supine position with mild neck extension were done skin sterilization and local anesthesia with 2% lidocaine at the needle-puncture site. We used an 18 gauge internally cooled monopolar electrodes (5mm or 7mm in active tips) which were connected to a radiofrequency generator (CoATherm AK- F200, APRO KOREA Inc.) to puncture into the nodule under US guidance via the trans-isthmic approach (Fig. 1A). The nodules were ablated by using the moving-shot technique (Fig. 1B). Hydro-dissection was used in a few cases to preventing important structures such as the nerve and artery by injecting slowly 5% dextrose (Fig. 1C). The transient hyperechoic zone proved nodules ablated completely [12, 19, 20]. In the case of the cystic nodule(s) or predominantly cystic nodule(s), fluid aspiration was performed completely before ablating the nodule and its vascularity. Patients were asked to stay in the hospital for 60 minutes after the procedure and discharged if having no complications.
Follow-up of the patients
Follow-up was performed at 1, 3 months after the treatment section. In the first month post-ablation, US evaluation, thyroid function tests (TSH, FT4), symptom score, and cosmetic score were evaluated. In other follow-ups, only US examination was used. Volume reduction rate (VRR) of the treated nodule was calculated based on the formula:
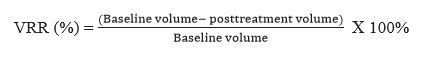
A > 50% volume reduction of the initial nodule volume measured at each follow-up US examination was considered as a therapeutic success [16]. Also, we recorded any specific complaints or concerns in the follow-up period.
Efficacy outcome
The primary endpoints were efficacy after 1 month and 3 months post-ablation through VRR. Therapeutic success was defined as a VRR > 50% of the initial nodule volume measured at each follow-up US examination [16]. Secondary endpoints were improvements in symptoms and cosmetic scores, no change of thyroid function tests.
Safety outcome
Safety outcome (complications and side effects) followed as reported by the international working group on image-guided tumor ablation [21]. Major complications include substantial morbidity and disability which increases the level of care, hospital admission, hemorrhage need a blood transfusion, and permanent voice change. Other complications were identified as minor complications (pain, transient voice change, vomiting, and skin burns) .
Demographic characteristics and other factors
In this study, demographic information included age (continuous variable), sex (categorical variable: male and female). Treatment characteristics included ablation time (continuous variable: minute), max RF power (continuous variable: Walt), min RF power (continuous variable: Walt), and volume of lidocaine used (continuous variable: ml).
Statistical analysis
SPSS version 20.0 for Windows was used for all statistical analyses. The number of events and their percentage were calculated as the safety outcome. To evaluating the RFA efficacy, which is a numeric outcome variable, our purpose is to calculate the mean and standard deviation (SD) of the VRR during the follow-up period (1 month and 3 months post-ablation). Although the scheduled examinations (1 month and 3 months after section treatment) were informed to patients, the included patients did not exactly follow this schedule due to individual reasons and COVID19, as a limitation of this study. A general linear model with 3 times repeated measurement was used to compare changes in nodule volume, largest diameter, symptom score, and cosmetic score from the initial time to 1 month, 3 months after the procedure. The Friedman test or the Wilcoxon’s matched-pair signed-rank test was used to alternating Paired t-tests to compare changes in volume reduction rate and therapeutic success rate from 1 month to 3 months after RFA if data cannot be assumed to be normally distributed. To identify factors that were independently predictive of efficacy (the volume reduction ratio at 3 months), we used multiple linear regression analysis. Variables entered into the model included age (continuous variable), sex (categorical variable: male and female), symptom score (continuous variable: range from 1–10 score), cosmetic score (continuous variable: range from 1–4 score), initial volume (continuous variable), thyroid functions (TSH, FT4 - continuous variable), characteristic of nodules (categorical variable: solid nodules, predominantly solid nodules, cyst), ablation time (continuous variable), max RF power (continuous variable), min RF power (continuous variable ), largest diameter (continuous variable) and volume of lidocaine used (continuous variable). Statistical significance was defined when the p-value was less than 0.05.