Methods And Materials
Study Area and setting
Ethiopia is situated in the northeastern part of Africa. It found between 30 and 150 north latitude and 330 and 480 east longitudes (40). It is bounded by six countries, namely: Eritrea, Djibouti, Kenya, Somalia, South Sudan and the Sudan, and the country covers an area of 1.1 million square kilometers ranging from 4,620m above sea level(41).The main climate type is tropical monsoon, with temperature climate on the plateau and hot in the lowlands. There are topographic-caused climatic variations broadly categorized into three: the “Kolla”, or hot low lands which are found up to approximately 1,500 meters above sea level, the “Wayna Degas” which ranges between 1,500-2,400 meters above sea level and the “Dega” or cool temperate highlands 2,400 meters above sea level. Ethiopia has a total of 114,963,588 populations; of this 18,394,194 are under-five children(41). The country has 20% of urban area, Government Expenditure on Health Care is 4 % of the total expenditure in the country.(42).
The global report on food crisis indicates that, Ethiopia’s GDP Per Capita purchasing power parity (PPP) in the country is US $1916.1 and it has a poverty rate of 29.6%. The Human Development Index (HDI) rank is 174 among 187 countries and there are 9.7 Million people who are food insecured in the country. About 85% of the population is dependent on Agriculture in Ethiopia(41). There is a fertility rate of 4.6, infant mortality rate of 48 (per 1,000 live births) and child mortality rate of 67 per 1,000 live births in the country (43).
Study design and study period
A cross-sectional study design using secondary data from 2016 EDHS was conducted from February to May.
Source and Study Population
The source population is all Ethiopian children aged 0–59 months, who are living with the contemporary respondent, while the 2016 EDHS are being conducted. The study population was children who are incorporated in the 2016 Ethiopia Demographic and Health Surveys.
Sample Size determination and sampling procedures
A total of 10,641children from EDHS 2016 were included from nine geographical regions and two administrative cities of Ethiopia. The sampling frame used for 2016 EDHS was the Ethiopian Population and Housing Census (EPHC), which was conducted in 2007 by the Ethiopia Central Statistical Agency (CSA) with Federal Ministry of Health (FMOH). The sampling frame contains information about the Enumeration areas (EA) location, type of residence (urban or rural), and estimated number of residential households. The samples for 2016 EDHS are designed to provide estimates of key indicators for the country as a whole, for urban and rural areas separately, and for each of the nine regions and the two administrative cities.
The 2016 EDHS sample was stratified and selected in two stages. Each region was stratified into urban and rural areas, which yielded 21 sampling strata. Samples of EAs were selected independently in each stratum in two stages. Clear stratification and proportional allocation was achieved at each of the lower administrative levels by sorting the sampling frame within each sampling stratum before sample selection, according to administrative units in different levels, and by using a probability proportional to size selection at the first stage of sampling.
From the first stage, a total of 645 EAs (202 in urban areas and 443 in rural areas) were selected in 2016 EDHS and with probability proportional to EA size (based on the 2007 PHC) and with independent selection from each sampling stratum for this recent survey. A household listing operation was performed in all of the selected EAs. The resulting lists of households served as a sampling frame for the selection of households in the second stage. In the second stage of selection, a fixed number of 28 households per cluster were selected with an equal probability systematic selection from the newly created household listing. Totally, 18,008 households were selected of which 17,067 are occupied. In all of the selected households, height and weight measurements will be collected from children aged 0–59 months, and women aged 15–49.The 2016 EDHS sample contained 18,008 households from 645 clusters, and 15,683 women aged 15–49 years were interviewed; the response rate was 95%.
Inclusion and exclusion criteria
Inclusion criteria: Children 0–59 months of age, complete data on diarrhea status and children with their mothers for measurements and completion of the questionnaires during survey.
Exclusion criteria: Children whose age is unknown, children who were not with their mothers/caregivers for and children diarrhea status for last two week before survey were not measured excluded from the study.
Study variables
Dependent variables was diarrheal status of the child (0-59months)
Independent variables
Individual level factors
Socio-Demographic and Economic characteristics of the family (household) include age of child, sex of child and wealth status. Under maternal and child related factors incorporate education level, maternal Age, child nutritional status, maternal or caregiver’s economical and educational status, hand washing practice during critical times, household wealth index, vaccination status of the child, child feeding practice, maternal employment status and maternal or caregiver’s diarrhea history. Community level factors were source of drinking water, unprotected water sources, improper disposal of wastes, family member size, toilet facilities, no of Children in household, place of residence and region.
Operational definition
Under Five Childhood Diarrhea: - It was defined as the presence or absence of UFCD during the last two weeks prior to this study(44).
Improved drinking water sources: - included piped water, public taps, standpipes, protected shallow wells, and springs.
Unimproved water sources: - were surface waters, unprotected shallow wells, and unprotected springs.
Improved latrines: - included any non-shared toilet, mostly flush toilets connected to piped sewer systems, septic tanks, and pit latrines, ventilated improved pit latrines, and pit latrines with slabs.
Unimproved latrines: - included the pour-flush type not connected to a sewer, pit latrines without a slab, open pits, and open defecation. Critical hand washing times were nominated as; before food preparation, eating, supplementary child feeding, and breastfeeding and after defecation and cleaning a child after defecation(43).
Vaccination status:- was considered fully vaccinated at 12 months, if the child had received the following vaccinations in the first year of life and have confirmed immunization card(45).
Appropriate child feeding practice:- Early initiation of breastfeeding within first hour of birth, exclusive breastfeeding for the first six months followed by continued breastfeeding for up to two years and beyond with appropriate complementary foods after completion of 6 months(46).
Family member size: - number of family member living with fewer than five children.
High birth order: -when the birth order duration is less than one year gab.
Data collection methods and Tools
Before extracting the data, permission was obtained from demographic health survey data center by persuading the purpose of the study. After getting permission, data were downloaded in Stata software data set form. Stata version 14 was used for cleaning and analysis of data.
For the purpose of this research, the under-five children data separately was received from central statistical agency by registered in it. The link was received and downloaded.
Data Processing and Analysis
Data cleaning was done to check for consistency and missing value. Recoding, labeling and exploratory analysis was performed. Categorization was done for continuous variables using information from different literatures and re-categorization was done for categorical variables accordingly. Model fitness was done by using Log likelihood, AIC, BIC and ICC. Sample weights were applied in order to compensate for the unequal probability of selection between the strata that are geographically defined, as well as for non-responses.
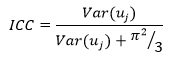
Multilevel analysis was conducted after checking that the data is eligible for multilevel analysis that means ICC greater than 10%. ICC calculation formula is as follows:
\(Var\left({u}_{oj}\right)\) : Is the community (cluster) level variance.
 : Is the standard logistic distribution, that is, the assumed individual variance?
: Is the standard logistic distribution, that is, the assumed individual variance?
Since DHS data are hierarchical, i.e., individuals (level 1) were nested with in communities (level 2), two-level mixed-effects logistic regression model was fitted to estimate both independent (fixed) effects of the explanatory variables and community-level random effects on childhood diarrhea.
Because the log of the probability of childhood diarrhea was modeled using two-level multilevel model as follows;\(log\left[\frac{{\pi }_{ij}}{1-{\pi }_{ij}}\right]={\beta }_{0}+{\beta }_{1}{\text{{\rm X}}}_{ij}+\dots {\beta }_{2}{\text{Y}}_{ij}+{u}_{j}+{e}_{ij}\)
Where, i and j are the level 1 (individual) and level 2 (community) units, respectively; X and Y refer to individual and community-level variables, respectively; \({\pi }_{ij}\) is the probability of childhood diarrhea for the ith under-five child in the jth community and \(1-{\pi }_{ij}\) is probability of under-five child don’t have diarrhea for the ith under-five child in the jth community(cluster). The β’s was the fixed coefficients. Whereas, β0 is the intercept-the effect on the probability of childhood diarrhea in the absence of influence of predictors; and \({ u}_{j}\) showed the random effect (effect of the community on childhood diarrhea) for the jth community and \({e}_{ij}\)showed random errors at the individual levels. By assuming each community had different intercept (β0) and fixed coefficient (β), the clustered data nature and the within and between community variations were taken in to account.
Bi-variable and multilevel logistic regression analysis was done and model fitness was checked. Those variables which had P-value less than 0.25 were candidates to build model 3 (model-3). After this analysis was performed, four models were constructed for this multilevel logistic regression analysis. The first model was an empty model or null model without any explanatory variables, to evaluate the extent of the cluster variation on diarrhea among under five children. The second model was adjusted for the individual-level variables; the third model can be adjusted for community (cluster) level variables while the fourth model was adjusted for both the individual and community level variables simultaneously.
The measures of association (fixed-effects) estimates the associations between likelihood of under-five children diarrhea and various explanatory variables were expressed as Adjusted Odds Ratio (AOR) with their 95 % Confidence level. A variable in which the confidence interval does not include the null value and p-value < 0.05 can be used to define statistical significance.
The measures of variation (random-effects) were reported by using intra-cluster correlation (ICC), Median Odds Ratio (MOR) and proportional change in variance (PCV). PCV was calculated to measure the variation between clusters. ICC was used to explain cluster variation while MOR is a measure of unexplained cluster heterogeneity (39).
The ICC shows the variation in under-five diarrhea due to community characteristics. The higher the ICC, the more relevant was the community characteristics for understanding individual variation in childhood diarrhea. The ICC was calculated as follows: [ICC = V/V + P2/3] where V is the estimated variance of clusters. MOR is defined as the median value of the odds ratio between the area at highest risk and the area at lowest risk when randomly picking out two areas and it was calculated using the formula [ MOR = exp (√2V + 0.6745) ≈ exp (0.95*V)]. In this study MOR shows the extent to which the individual probability of under-five diarrhea is determined by residential area. The proportional change in variance (PCV) measures the total variation attributed by individual level factors and area level factors in the multilevel model.
The variability on the odds of childhood diarrhea explained by successive models was calculated by Proportional Change in Variance (PCV) as:
\(PCV=\frac{{V}_{e}-{V}_{mi}}{Ve}\) , Where,
\({V}_{e}\) : is the variance in childhood diarrhea in the null model
\({ V}_{mi}\) : The variances in the successive models.
The presence of Multicollinearity was checked among independent variables using standard error at cut off point of ± 2. Log likelihood test and AIC (Akakian Information Criteria) was used to estimate the goodness of fit of the adjusted final model in comparison to the preceding models (individual and community level model adjustments). The log likelihood value for each subsequent model was compared and the model with the highest value was considered to be the best fit model. On the contrary, the model with the lowest AIC was the best.
Data quality assurance
For 2016 EDHS pretest containing in-class training, biomarker training, and field practice days were conducted. The field practice was conducted in clusters around Bishoftu which were not included in the 2016 EDHS sample. A total of 60 trainees attended this pretest. Following the field practice, a debriefing session was held with the pretest field staff, and modifications to the questionnaires were made based on lessons drawn from the exercise. CSA recruited and trained 294 people for the main fieldwork who were to be engaged as team supervisors, field editors, interviewers, secondary editors, and reserve interviewers. The training was conducted from December 14, 2015, to January 17, 2016, at Debre Zeit Management Institute in Bishoftu. The training session consisted of instruction regarding interviewing techniques and field procedures, a detailed review of questionnaire content, instruction on how to administer the paper and electronic questionnaires, mock interviews between participants in the classroom, and practice interviews with real respondents in areas outside the survey sample. Data quality management during the recent EDHS survey was published (43). An Initial exploratory analysis was conducted to check for outliers, missing and consistency of dataset.
Result writing and dissemination plans
The result of the study will be written and presented to Debre Berhan University, College of Health Sciences, and Department of Public Health. The finding of this study will be disseminated timely to all relevant stakeholders that may concern themselves. It will be sent for publication in scientific journal, and online dissemination will be taken into account. Presentations on different occasions will be made on various seminars, workshops and scientific conferences.
Ethical consideration
Ethical clearance was obtained from the Ethical Review Committee of Debre Berhan University, College of Health Sciences with approval and supporting letter. Authorization letter of permission for downloading 2016 EDHS dataset was obtained from CSA of Ethiopia, by requesting with the website https;//dhsprogram.com/data/terms-of-use.cfm with the help of ICF international. All data was treated as confidential and no need to identify any household or individual respondent interviewed in the survey.