Methods
Study area and period
Addis Ababa, capital city of the Federal Democratic Republic of Ethiopia, located at the center of the country that had 10 sub-cities and 116 Woredas with a total population of around 3.4 million according to Ethiopian population projection for all regions in Wereda level from 2014–2017 (9). Its area was estimated to be 530 Km2 with altitude ranging from 2200 to 3000 meter above sea level, average temperature of 22.8 °C and average rainfall of 1,180.4 mm3. Addis Ababa had 53 hospitals of which 13 were public and 40 were private. Setting of study were in four randomly selected hospitals from Addis Ababa public hospitals of Ethiopia; which were Tikur Anbessa Specialized Hospital (Black Lion Specialized Hospital) had a total of 646 inpatients from this 374 were adult inpatients, St.paulos hospital had total of 502 inpatients from this 237 were adult inpatients, Yikatit 12 hospitals had a total of 359 inpatients from this 139 were adult inpatients and Zewuditu hospitals had a total of 208 inpatients from this 72 were adult inpatients at a time. The study was conduct from March1 to 30, 2020.
Study design-An institution based cross - sectional study design was used.
Source population- All hospitalized medical surgical adult inpatients at selected public hospitals.
Study population- Randomly selected hospitalized medical surgical adult inpatients available during the study period and who fulfilled the inclusion criteria.
Inclusion criteria- All medical surgical inpatients greater than or equal to 18 years old present during data collection.
Exclusion criteria- Medical surgical adult inpatients unable to communicate with critical illnesses, physical impairment to speech, mental disability and post anesthesia were excluded.
Sample size determination-The sample size was calculated by using single population proportion formula, considering the following assumptions; prevalence of mental distress 58.6% which done in Gondar University hospitals among medical surgical adult inpatients,95% confidence interval and 5% margin of error (10).
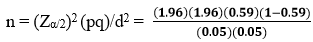 = 372 with 10% non-response rate the total sample size were 408.
= 372 with 10% non-response rate the total sample size were 408.
Four hospitals selected using of simple random sampling lottery method, which were TASH (Tikur Anbessa Specialized Hospital), St.paulos hospital, Yikatit hospital and Zewuditu hospital and a total of 408 study subjects were selected from 822 reference population using systematic random sampling every k = 2 interval.
Study variables
The dependent variable was mental distress and the independent variables included sociodemographic factors (age, sex, religion, ethnicity, residence, occupation, monthly income, marital status, education status), Substance use related variables (tobacco use, alcohol use, chat use, illegal drug use), Psychosocial variables (social support, living condition), clinical related variable (previous psychiatric history, psychiatric illness after admission, psychiatric consultation, family history of psychiatric illness, previous hospital admission, ward admitted, comorbidity, hospital stay).
Data collection tool and procedure
Amharic version of the questionnaire was used for data collection. First the questionnaire was prepared in English language then translated to Amharic and back to in English. Two clinical staffs as supervisor and four nursing students as a data collector with half day time training were used. Self-Reporting Questionnaire; dichotomous type scale to determine the prevalence of mental distress in adult inpatients. The SRQ-25 was a standardized questionnaire having 25 item questions adapting the SRQ for Ethiopian Populations for culturally-sensitive psychiatric screening instrument. This tool was validated in Ethiopia and other low socioeconomic countries. In Ethiopia, sensitivity of 86% and specificity of 84% with a cut-off point of 8 (11).
Data processing and analysis
First the data was checked for its completeness and consistency, and then it was coded and entered in EPI data version 3.02 software. After entry, data was exported to statistical package for social science (SPSS) version 26 for analysis. Descriptive analysis using frequencies, proportions, graphs was performed to describe number and percentage of socio-demographic characteristics of the sample and other variables. Binary logistic regression analyses model was used to identify associated factors of mental distress. This was done by odds ratio and p value with 95% confidence interval (CI). Explanatory variables with p-value ≤0.25 in the bivariate logistic regression was entered into multivariate logistic regression analysis to control possible confounding. Hosmer-Lemeshow’s test was found to be insignificant (p-value = 0.999) and Omnibus tests was significant (P-value = 0.001) which indicate the model was fitted. P-value of less than 0.05 was used to declare level of statistically significant and adjusted odd ratio (AOR) with 95% CI was estimated to identify significantly associated variables with the dependent variable, mental distress. Finally, the results were presented in text, tables and graphs based on the types of data.