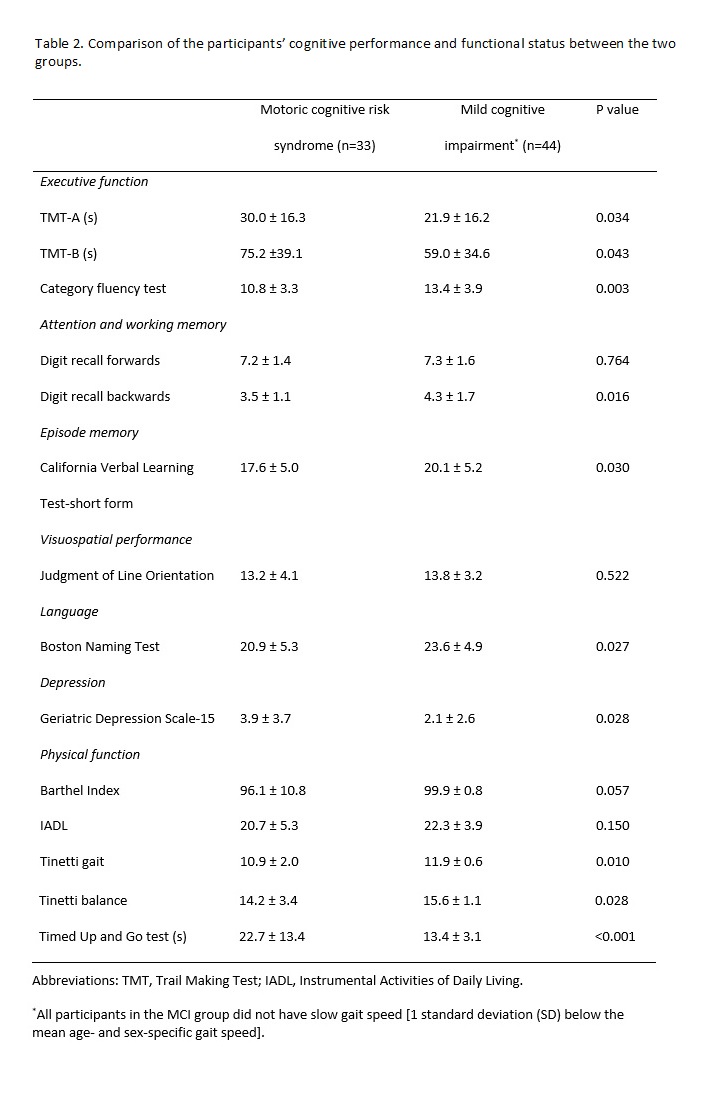
In the present study, it was demonstrated that compared to individuals with MCI but without MCR syndrome, subjects with MCR are more likely to exhibit executive function, attention, memory, and language impairments. Our results also showed that physical functions, including gait and balance performance, are significantly lower in people with MCR than in those with MCI but without MCR syndrome. To the best of our knowledge, this is the first study to compare cognitive performance and physical function in individuals with two types of cognitive impairment, MCR and MCI. We also found that executive function is the primary factor associated with gait speed compared with attention, memory, visuospatial, and language performance.
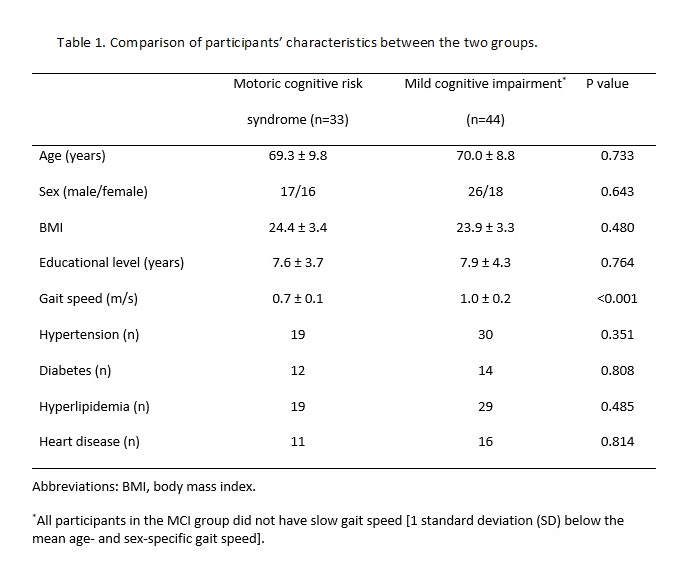
A major contribution of this study to the literature includes the results of cognitive performance and physical function in individuals with MCR versus those with MCI but without MCR syndrome. Recent reports have shown that the simultaneous presence of cognitive decline and a slow walking speed can predict dementia [19, 20]. MCR is a novel concept and is defined as a heterogeneous clinical manifestation characterized by the simultaneous presence of an objectively slow gait speed and subjective cognitive complaints [21, 43]. Individuals with MCI demonstrate cognitive impairment with minimal impairment in IADL [44]. Both conditions are linked to poor cognitive function and represent a stage of predementia [22]. However, currently, the information on the characteristics of MCR and the differences between MCR and MCI are still limited. In the present study, we found that compared to MCI but without MCR, MCR is linked not only to poorer physical function but also to poorer cognitive performance in tasks related to executive function, attention, working memory, episode memory, and language. This result indicates that compared with MCI but without MCR, MCR might lead to more severe overall functional deterioration in older adults. In a three-year longitudinal study, people with MCR were found to be at higher risk of developing dementia than were people with not MCR (hazard ratio: 3.27) [21]. A random effects meta-analysis reported that the relative risk of dementia was 3.3 in those with MCI versus age-matched controls 2-5 years later [45]. Although the conversion rates in these two groups are similar, the research designs and the participants included in these studies differed greatly. Since we found significant differences in cognitive performance and physical function between MCR and MCI patients, it is important that a large cohort study is conducted in the future to compare the rate of conversion to dementia between these two groups.
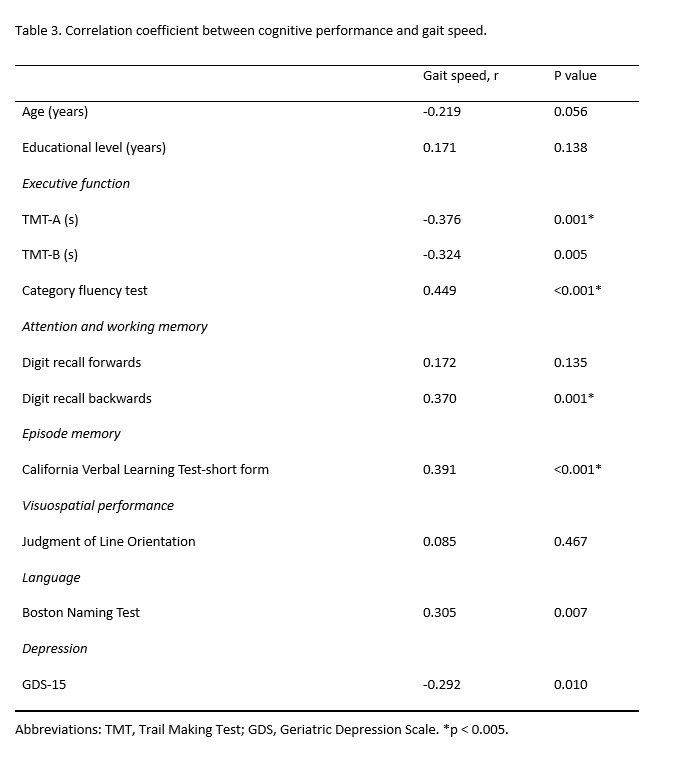
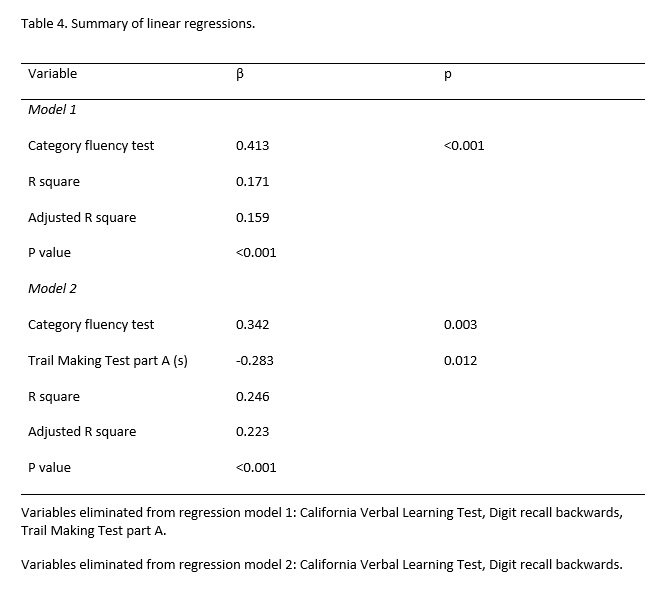
Based on the definitions of MCR and MCI, both are predementia cognitive disorders, and the factor that differentiates them is gait speed. Walking is a very common activity of daily living and is a consequence of multifactorial and multisystem (sensory, musculoskeletal, nervous, and cardiorespiratory) coordination. Executive function [16, 46] and attention [46, 47] are considered to be the most important cognitive domains affecting gait performance. Our research findings reported that people with MCR who had a slower gait speed also had poorer executive function, poorer attention and memory performance, poorer language function, and more depressive symptoms than did participants with MCI but without MCR syndrome. In addition, we also noted that executive function was the primary factor associated with gait speed compared with other domains of cognition, which is consistent with other research results [48, 49]. A growing body of evidence suggests that frontal subcortical circuits mainly control the speed of walking [50]. Moreover, compromised frontal lobe white matter was found to be associated with executive network functional impairments and slower walking speeds in elderly individuals [51, 52]. These brain areas are highly susceptible to white matter hyperintensities, microvascular damage, and neurodegenerative pathologies, which are common precursors of dementia [52]. In summary, brain regions and networks specifically control both higher-level cognitive function and gait performance and explain the relationship between a slow walking speed and dementia pathologies.
Regarding physical function, our results showed that the mean Tinetti Assessment Scale score in subjects with MCR was significantly lower than that in people with MCI but without MCR, indicating that individuals with MCR not only walk slowly but also have poor balance. Moreover, compared to the MCI group, the MCR group needed more time to complete the TUG test (mean, MCI group=13.4 seconds; MCR group=22.7 seconds, p<0.001). The TUG test is a reliable measure of functional activity that captures transfers, straight walking, and turning movements [53]. It has been reported that this test can be used to identify elderly individuals who are prone to falls (completion time of ≥ 14 seconds), with a sensitivity of 0.87 and a specificity of 0.87 [54]. This result demonstrates that our MCR group had a high-risk for falling, which is consistent with other research results [24]. As mentioned above, maintaining a normal well-balanced gait is a complex process requiring the efficient cooperation of multiple systems, such as those controlling motor, cognitive, and sensory processes [16, 20, 55], and the inability to have a normal gait can lead to falls. We therefore suggest that MCR is an effective screening tool for the risk of falls in older populations.
According to our results, people with MCR have poorer cognitive function and physical function than do MCI but without MCR patients, indicating that MCR might lead to more severe overall functional deterioration than MCI in older adults. Previous study indicated that slowing gait occurs approximately a decade prior to MCI onset[56] MCR does not require a time-consuming comprehensive neuropsychological assessment, unlike MCI, which is convenient for the clinical evaluation of the risk of dementia in community-dwelling older populations. In addition, compared with people with MCI, people with MCR might have a higher risk of falling, based on the completion time for the TUG test. There are some study limitations that should be addressed in the present study. The inclusion of a relatively small number of participants and the enrollment procedure of participants prioritizes the MCR syndrome made it impossible to perform any subgroup analyses with sufficient power, such as an MCI subtype comparison. Studies with a larger sample size should be conducted in the future to confirm our results and to conduct subgroup analyses. Besides, previous study indicated that slowing gait occurs approximately a decade prior to MCI onset[56], which suggests that the diagnosis of MCR, based on slow gait speed and subjective cognitive complaints, might precede the diagnosis of MCI. However, our result supported the direct opposite, which might be related to the enrollment procedure with a priority for the MCR group and the recruitment place was in the medical center. The elderly with subjective cognitive complaints who came to the medical center were usually in more serious condition than the elderly in the community. Future research should expand the enrollment of participants to the elderly in the community. We also used a cross-sectional study design, which prevented us from investigating changes in cognitive and physical function in the two groups over time. To better understand the actual interaction between cognitive and physical functions in aging populations that are at high risk of dementia, a large cohort study is warranted and encouraged. Moreover, it should be noted that since MCR is defined as a condition characterized by a slow gait speed in the presence of subjective cognitive complaints in elderly people not diagnosed with dementia or mobility impairments, the MCR subjects included in this study may or may not have met the MCI diagnosis. In this study, we did not exclude MCR subjects with MCI, which may have affected our results. However, the definition of MCR does not include conditions that can exclude subjects with MCI [21]. Therefore, the characteristics and differences between MCI and MCR need further clarification.