The flow diagram of the search strategy is summarized in Fig. 1. Initially, 551 articles on the comparative study of OLF and TLIF were searched in the electronic database. The remaining 25 studies were read in full, and 16 studies were excluded due to unavailable selection criteria. Finally, a total of nine articles that involved 593 patients (271 patients in the OLIF group and 322 patients in the TLIF group) met the inclusion criteria, and were included in the present meta-analysis [6–14]. Among the included articles, six articles were in the English language, while the other articles were in the Chinese language.
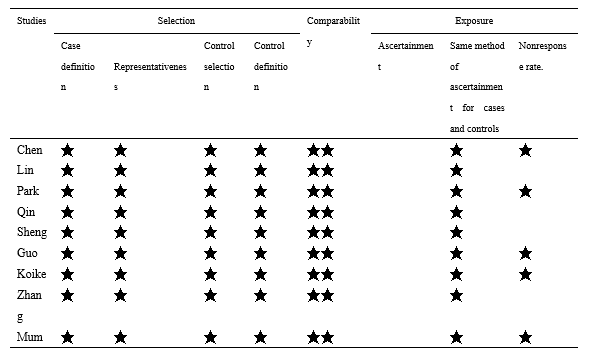
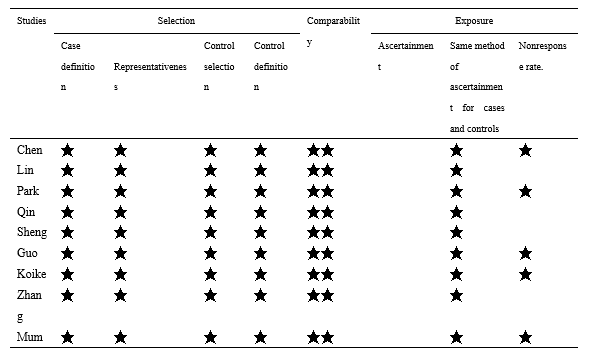
The characteristics of the included studies are presented in Table 1. The bias risk and quality of the included studies were assessed using the Newcastle-Ottawa Scale (NOS). The NOS contains eight scoring items categorized into three fields: Selection, Comparability, and Outcome. The full score was 9, and studies that achieved a score of 6 or more were considered as high quality. Among these studies, five studies scored 8 points, while the remaining studies scored 7 points. These studies are of high quality, as presented in Table 2.
Table 2. Newcastle-Ottawa scale
Operation Time
The data of eight studies, which included 513 patients (242 patients in the OLIF group and 271 patients in the TLIF group) was analyzed. The pooled estimate revealed that there was a statistical difference between both groups, in terms of operative time, in favor of the shorter operative times for the OLIF group. [SMD=-1.29, 95% CI (-2.12,-0.47), P<0.05; Fig. 2]. This meta-analysis involved a random-effects model due to the high heterogeneity among the studies (I2 = 94%).
Estimated Blood Lose
The estimated blood loss obtained in eight studies that involved 513 patients (242 patients in the OLIF group and 271 patients in the TLIF group) was analyzed. The result of the meta-analysis indicated that the TLIF group had a significantly higher estimated blood loss, when compared to the OLIF group, with significant heterogeneity [P<0.00, MD=-141.09 (-183.44, -98.74); I2 =97%; Fig. 3].
Hospital Stay
Three studies, which included 211 patients (97 patients in the OLIF group and 114 patients in the TLIF group), reported the data on hospital stays. The meta-analysis results revealed that TLIF required a significantly longer hospital stay, when compared to OLIF [P<0.05, SMD=-1.72 (-3.29, -0.15)]. This meta-analysis involved a random-effects model due to the high heterogeneity among studies (I2 =70%). The details for each study are shown in Figure 4.
ODI
Among the nine articles, six studies compared the ODI. The forest plot for the ODI between OLIF and TLIF is presented in Figure 4. The meta-analysis indicated that OLIF was superior to TLIF, but the difference was not statistically significant [P=0.40, MD=-0.52 (-1.73, -0.69); Fig. 5], with a detected significant heterogeneity (I2=79%; P=0.0002).
VAS
Six of nine included studies involved the VAS. The forest plot for the VAS between OLIF and TLIF is shown in Figure 5. The combined results suggest that the score of VAS in the OLIF is lower than that in the TLIF, but there was no significant difference [P=0.67, MD=-0.01 (-0.34, -0.22)]. Evidence of statistically significant heterogeneity was observed [I2 =83%, P<0.0001; Fig. 6].
Radiographic Results
The investigators also compared the intervertebral disc height, foramen height, fusion rate, lumbar lordosis Angle and intervertebral disc angle between the two groups after the operation. A total of five component studies, which included 407 patients (190 patients in the OLIF group and 217 patients in the TLIF group), provided the value of the disc height. Disc height in the OLIF was similar to that in the TLIF [MD=1.17, 95% CI (0.29-2.05), P=0.009; I2=91%; Fig. 7]. Four studies, which involved 196 patients (97 patients in the OLIF and 99 patients in the TLIF), investigated the data for the lumbar lordosis angle. Compared with OLIF group, the TLIF group was associated with a much more improved lumbar lordosis angle after the operation, with no statistical difference and significant heterogeneity [MD=2.18, 95% CI (-1.49~5.85), P=0.24; I2=87%; Fig. 8]. Four studies, which included 337 patients, compared the effects of OLIF and TLIF on the disc angle. The TLIF had a greater recovery of the disc angle than that of the OLIF, but there was no significant difference with large heterogeneity between groups [MD=5.33, 95% CI (-0.92~11.58), P=0.09; I2=98%; Fig. 9]. Three studies, which included 288 patients, reported the data on the fusion rate. The meta-analysis results revealed that the postoperative fusion rates were similar between the two groups, but there was no statistical difference [MD=1.55, 95% CI (-0.47-5.1), P=0.09; Fig. 10]. This meta-analysis involved a random-effects model due to the high heterogeneity among studies (I2=67%). A total of 321 patients from four studies compared the recovery of the foramina height between OLIF and TLIF. The combined data revealed that the recovery of the foramina height in the OLIF was higher than in the TLIF, but there was no statistical difference [MD=-0.10, 95% CI (-0.19 ~ -0.00), P=0.05; I2 = 0%; Fig. 11].